DM1 and DM2 are genetic disorders characterized by progressive muscle wasting and weakness, impacting multiple body systems. Understanding their distinct genetic mutations and symptoms is crucial for accurate diagnosis and management. This infographic visually breaks down the key differences and shared features of these myotonic dystrophies.
Understanding Diabetes: DM1 vs DM2
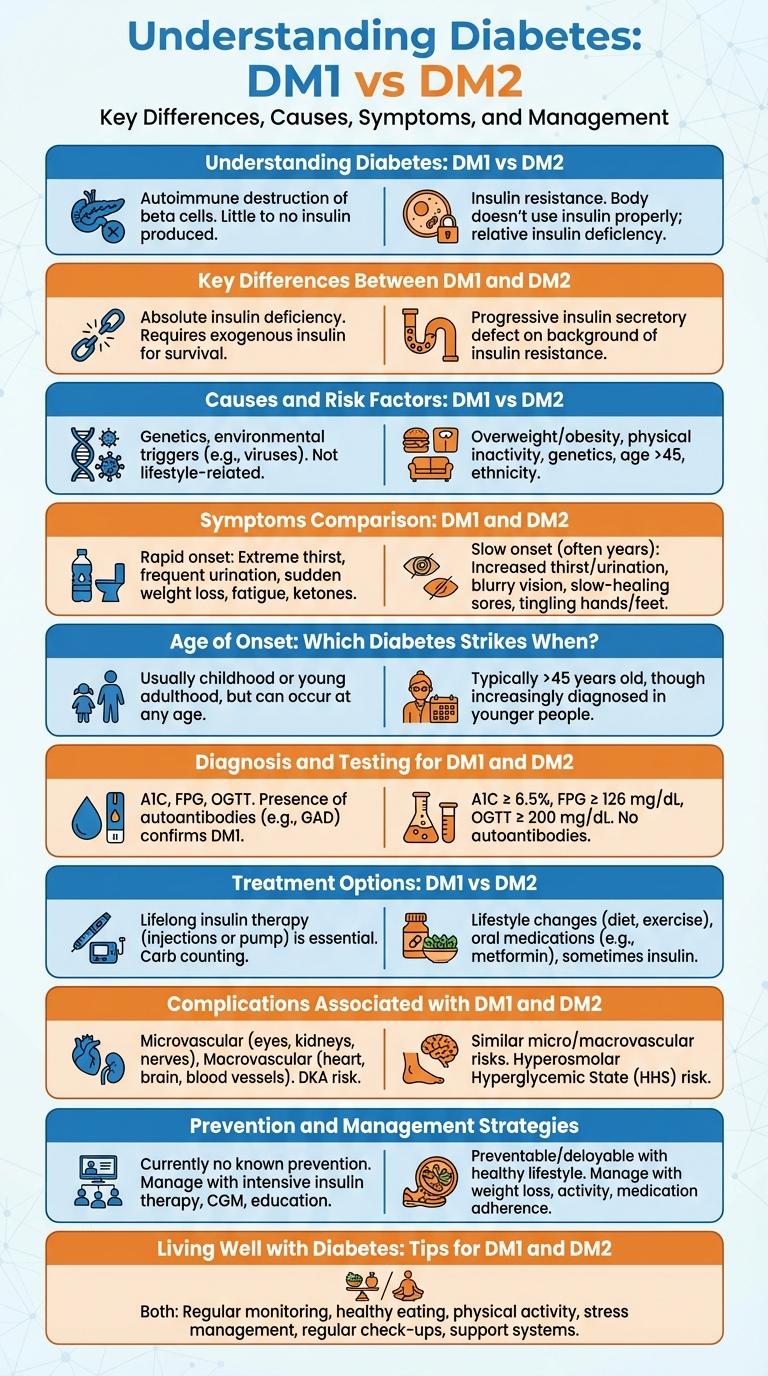
Diabetes Mellitus Type 1 (DM1) and Type 2 (DM2) are two distinct forms of diabetes affecting blood sugar regulation. DM1 commonly develops in childhood, while DM2 usually occurs in adults but is increasingly seen in younger populations.
DM1 is an autoimmune condition where the pancreas produces little or no insulin, requiring daily insulin therapy. DM2 results from insulin resistance and often develops gradually due to lifestyle and genetic factors. Managing DM2 may involve lifestyle changes, oral medications, and sometimes insulin.
Key Differences Between DM1 and DM2
Diabetes Mellitus Type 1 (DM1) and Type 2 (DM2) are both chronic conditions that affect blood sugar regulation but differ significantly in causes and management. Understanding the key differences between DM1 and DM2 is essential for accurate diagnosis and effective treatment.
- Cause - DM1 is an autoimmune disorder leading to insulin deficiency, whereas DM2 primarily results from insulin resistance combined with relative insulin deficiency.
- Age of Onset - DM1 commonly develops in children and young adults, while DM2 typically occurs in adults over 40 but is increasingly seen in younger populations.
- Insulin Dependency - People with DM1 require lifelong insulin therapy, while many with DM2 manage blood sugar through lifestyle modifications and oral medications before insulin is needed.
- Prevalence - DM2 is more prevalent globally, accounting for approximately 90-95% of diabetes cases, in contrast to DM1, which represents about 5-10% of cases.
- Symptoms Onset - DM1 symptoms usually appear abruptly, whereas DM2 symptoms develop gradually and may remain unnoticed for years.
Causes and Risk Factors: DM1 vs DM2
What are the primary causes and risk factors of DM1 versus DM2? DM1 is caused by an autoimmune destruction of insulin-producing beta cells, leading to absolute insulin deficiency. DM2 results from insulin resistance combined with a relative insulin deficiency, often influenced by lifestyle and genetic factors.
Symptoms Comparison: DM1 and DM2
Diabetes Mellitus Type 1 (DM1) primarily presents with sudden onset symptoms such as excessive thirst, frequent urination, and unexplained weight loss. Diabetes Mellitus Type 2 (DM2) often develops gradually, characterized by symptoms like increased hunger, blurred vision, and slow healing of wounds. Both types share symptoms like fatigue and frequent infections, but DM2 is more associated with insulin resistance and obesity.
| Symptom | DM1 vs DM2 |
|---|---|
| Onset | Sudden in DM1, gradual in DM2 |
| Weight Changes | Unexplained weight loss in DM1, often overweight or obese in DM2 |
| Thirst and Urination | Excessive in DM1, variable in DM2 |
| Hunger | Not typical in DM1, increased in DM2 |
| Wound Healing | Normal in DM1, slow in DM2 |
Age of Onset: Which Diabetes Strikes When?
| Diabetes Type | Age of Onset |
|---|---|
| Type 1 Diabetes (DM1) | Commonly diagnosed in childhood or adolescence, typically before age 20 |
| Type 2 Diabetes (DM2) | Usually develops in adults over 40, but increasingly seen in younger populations including teens |
| DM1 Onset Pattern | Rapid onset with symptoms developing over weeks |
| DM2 Onset Pattern | Gradual onset with symptoms appearing slowly over years |
Diagnosis and Testing for DM1 and DM2
Diagnosis and testing for Diabetes Mellitus Type 1 (DM1) and Type 2 (DM2) involve specific clinical evaluations and laboratory assessments to accurately distinguish between the two conditions. Early detection and precise diagnosis are essential for effective management and treatment planning.
- Autoantibody Testing in DM1 - Presence of autoantibodies such as GAD65 and IA-2 indicates autoimmune destruction of pancreatic beta cells in DM1.
- Fasting Plasma Glucose Measurement - Elevated fasting blood sugar levels above 126 mg/dL on two separate occasions suggest diabetes mellitus.
- Oral Glucose Tolerance Test (OGTT) - A 2-hour glucose level exceeding 200 mg/dL during OGTT confirms diabetes diagnosis for both DM1 and DM2.
Treatment Options: DM1 vs DM2
Treatment options for Diabetes Mellitus Type 1 (DM1) and Type 2 (DM2) differ significantly due to their distinct pathophysiologies. Understanding these differences is critical for effective disease management and patient outcomes.
- Insulin therapy in DM1 - Lifelong insulin injections are mandatory because the pancreas produces little to no insulin in DM1 patients.
- Oral medications in DM2 - Many DM2 patients manage blood sugar using oral hypoglycemic agents like metformin before progressing to insulin.
- Lifestyle modifications - Both DM1 and DM2 benefit from diet control and regular physical activity to optimize glucose control.
Tailoring treatment to the diabetes type improves glycemic control and reduces complications effectively.
Complications Associated with DM1 and DM2
Diabetes Mellitus Type 1 (DM1) and Type 2 (DM2) both lead to serious complications affecting multiple organ systems. Common complications include cardiovascular disease, neuropathy, nephropathy, retinopathy, and delayed wound healing. Effective management and early detection of these complications are essential to prevent severe outcomes and improve quality of life.
Prevention and Management Strategies
Diabetes Mellitus Type 1 (DM1) and Type 2 (DM2) require tailored prevention and management strategies to reduce complications. Effective approaches focus on lifestyle, medication, and regular monitoring.
For DM1, prevention is limited, but management includes insulin therapy and blood glucose monitoring. For DM2, prevention emphasizes healthy diet, regular exercise, and weight control, while management often adds oral medications and glucose tracking.
